Gestational Diabetes: Risks, Prevention, and Management During Pregnancy
What is Gestational Diabetes
Gestational diabetes is a type of diabetes that develops during pregnancy. It occurs when the body is unable to produce enough insulin to meet the increased demands of pregnancy. Insulin is a hormone that regulates blood sugar levels. During pregnancy, the placenta produces hormones that can interfere with insulin function, leading to elevated blood sugar levels. According to the American Diabetes Association, about four percent of pregnant women develop gestational diabetes. It is estimated that there are about 135,000 cases of gestational diabetes every year in the United States.
Development and Impact
Gestational diabetes usually develops around the 24th week of pregnancy and typically resolves after giving birth. However, it’s important to manage gestational diabetes because it can lead to complications for both the mother and the baby if left untreated. Complications may include macrosomia (a condition where the baby grows larger than usual), preterm birth, preeclampsia (high blood pressure during pregnancy), and an increased risk of type 2 diabetes for both the mother and the child later in life.
Causes and Effects
In most cases, women who develop gestational diabetes will not develop Type II diabetes. This is a condition affected by the pregnancy and the inability of the mother to use the insulin naturally developed in her body. It is caused by hormones triggered by the pregnancy and causes the mother to become insulin-resistant. Gradually, the mother develops high blood glucose levels, referred to as hyperglycemia.

Normally, a woman with gestational diabetes will be treated for the condition while pregnant. While there are no birth defects associated with this sort of illness as there are with women who have had diabetes before being pregnant, there is generally not a large cause for alarm for the child. However, if the condition is left untreated, it can hurt the baby. Because the mother is not getting rid of her excessive blood glucose, the child is getting more than his or her share of energy and fat. This often results in macrosomia. Macrosomia is simply the clinical name for a fat baby.
While some people think a fat baby is a sign of a healthy baby, a child born too fat may have a problem fitting through the birth canal. This can cause shoulder damage and may require a cesarean section birth. In addition, babies who are born obese can develop breathing problems and, if they remain obese, may themselves develop Type II diabetes.
Treatment and Management
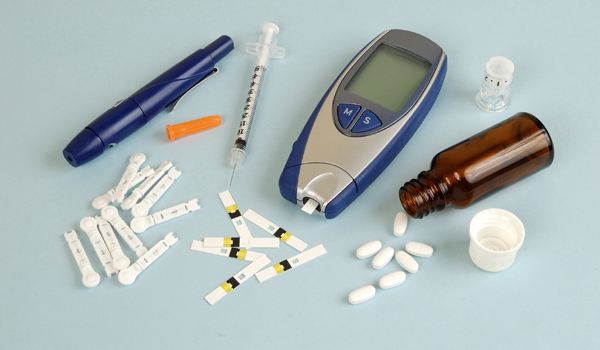
Fortunately, there is treatment for gestational diabetes. Insulin injections are usually given to the mother to keep the blood glucose levels intact. A woman who is planning on becoming pregnant, however, can avoid the complication of developing gestational diabetes before becoming pregnant.
Some of the ways a woman can do this is to lose weight if she is already overweight before becoming pregnant, develop a healthy exercise routine and follow certain food guidelines. The Glycemic Index is an ideal tool for a woman who is thinking about becoming pregnant to use to determine which foods to avoid. The Glycemic Index was developed for diabetics to categorize carbohydrates for those with diabetes.
When you become pregnant, follow the advice from your doctor regarding diet and exercise as well as any carbohydrate diets. Before becoming pregnant, discuss any concerns you have regarding weight or diabetes with your physician as he or she can probably give you some advice on how to avoid this pregnancy complication.
Even if you are diagnosed with gestational diabetes, chances are that you will not develop Type II diabetes, neither will your baby, and both of you will be just fine. Gestational diabetes is not a reason to panic. There is plenty of care available for women with this condition. Just be sure to follow any instructions given to you by your doctor.